Following the recent update to the National Institute of Care Excellence (NICE) guidelines for asthma care and management, Bedfont® Scientific Limited sponsored an informative webinar by Intermedical (UK) Limited. The session was led by experienced respiratory nurse Carol Stonham MBE, who discussed the guideline changes in detail and the vital role of Fractional exhaled Nitric Oxide (FeNO) testing in the asthma pathway.
As the first part of a three-part series on this insightful webinar, this article focuses on the foundations: patient-centered care, adjustments in diagnostic criteria, and the value of structured clinical assessments.
While typical guideline updates involve small adjustments to recommendations, this update represents a major shift in the diagnosis and management of asthma. This article examines the guidelines and their implications for FeNO.
The first recommendation, which healthcare professionals (HCPs) must be aware of and follow, is that healthcare should be patient-centered. Patients should be given sufficient time and information to make knowledgeable decisions regarding their care. Unfortunately, this can be challenging if the areas in which the HCPs work have a restrictive formulary.
How asthma is diagnosed
Firstly, as an HCP, a clear and thorough history should be taken to ensure asthma is suspected before testing. It is easy to observe a cough or a wheeze, but these alone should not lead to a diagnosis.
The recommendation has changed from HCP-reported wheeze to just “reported wheeze”. This should be treated with caution, as a patient's interpretation of a wheeze may differ significantly from an HCP’s interpretation.
- While symptoms such as cough, noisy breathing, and chest tightness are associated with asthma, it is important to remember that they should vary. This means the symptoms are not the same every day; variation may relate to time of day or time of year, for example.
- Patients should be able to identify triggers, such as “my symptoms are worse when I move from warm to cold environments”.
- HCPs should inquire about a family history of atopic disorders and ensure that symptoms have no alternative causes. All other possibilities should be ruled out before an asthma diagnosis is made.
The Quality and Outcomes Framework (QOF) had previously required more than one objective test for an asthma diagnosis, while the British Thoracic Society (BTS) and the Scottish Intercollegiate Guidelines Network (SIGN) allowed diagnosis without supportive testing.
The new joint guideline from NICE/BTS/SIGN introduces clarity and consistency to asthma diagnosis, allowing a diagnosis to be made with a suggestive clinical history and just a single supportive objective test, making the process simpler for HCPs to follow.
As mentioned in the previous guideline, once an asthma diagnosis is established, the HCP must record how that diagnosis was reached. This is a crucial step, as if the patient does not respond to treatment later on, the HCP can revisit the diagnosis and check the process to ensure accuracy.
What should be done with patients who are presenting?
Typically, two groups of people present in primary care: patients who appear well and claim to feel fine but mention occasional wheeze and chest tightness, and patients who present with active symptoms, where exploring their history reveals the issue has been longer-standing, with something causing an exacerbation.
The guidelines mandate treatment if patients are acutely unwell at presentation. Sending them away without treatment while waiting for tests may be unsafe. If feasible, a test should be conducted at that moment. However, if the patient does not feel well enough to undergo a test or the tests are unavailable, treatment should be initiated immediately, with tests performed as soon as possible. However, it is recognized that test results could return to normal due to treatment.
The guideline recommends the following tests for asthma diagnosis:
- Blood eosinophils
- FeNO test
- Spirometry
- Peak flow with bronchodilator reversibility (BDR)
Ideally, the test should be performed immediately, choosing the fastest and easiest option for the patient. Generally, tests such as spirometry and peak flow are challenging to perform when the patient is unwell, making a FeNO test the most suitable option.
Patient examination
During examination, HCPs should listen for the classic expiratory polyphonic wheeze. This symptom is specifically observed in asthmatic patients during exhalation. However, patients presenting well who have reported feeling unwell may not exhibit this wheeze, which should not rule out an asthma diagnosis, so testing should be performed.
Test sequence
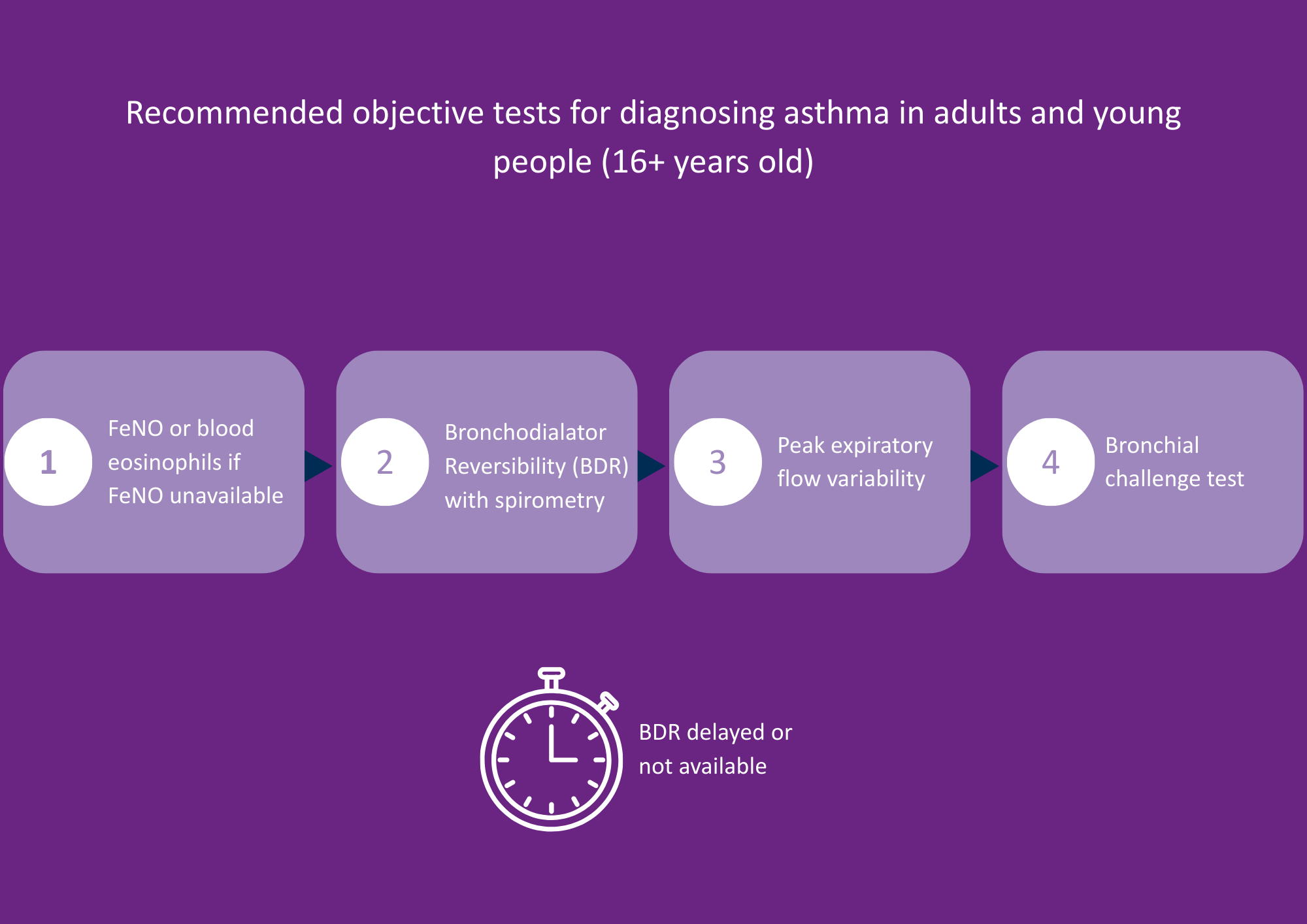
Image Credit: Bedfont® Scientific Ltd
After carrying out a clear history and a physical examination, if asthma is suspected, testing may begin.
Blood eosinophils or FeNO is the first-line test for adults and young people aged 16 and above. While blood eosinophils may be considered appropriate for adults, a follow-up appointment is required to discuss the results. It is possible to look up previous blood test results; however, many individuals, particularly young people, do not undergo regular blood testing, so this information may not be available.
Primary care is usually short on time, making a FeNO test the quickest test option, if available. The test is fast and easy, non-invasive, and can be conducted within the same appointment.
- If blood eosinophils or FeNO results suggest asthma, additional testing is not required, as an asthma diagnosis can be made.
- If these results do not suggest asthma, the next step is BDR with spirometry. The guidelines acknowledge that spirometry is not widely available, so if access to this test is delayed, HCPs can move on to a peak flow diary.
- If these subsequent tests do not suggest asthma, the next step is a bronchial challenge. However, this is a last-line investigation and should not be performed in primary care. A bronchial challenge test carries a high risk and should only be conducted with immediate access to resuscitation facilities.
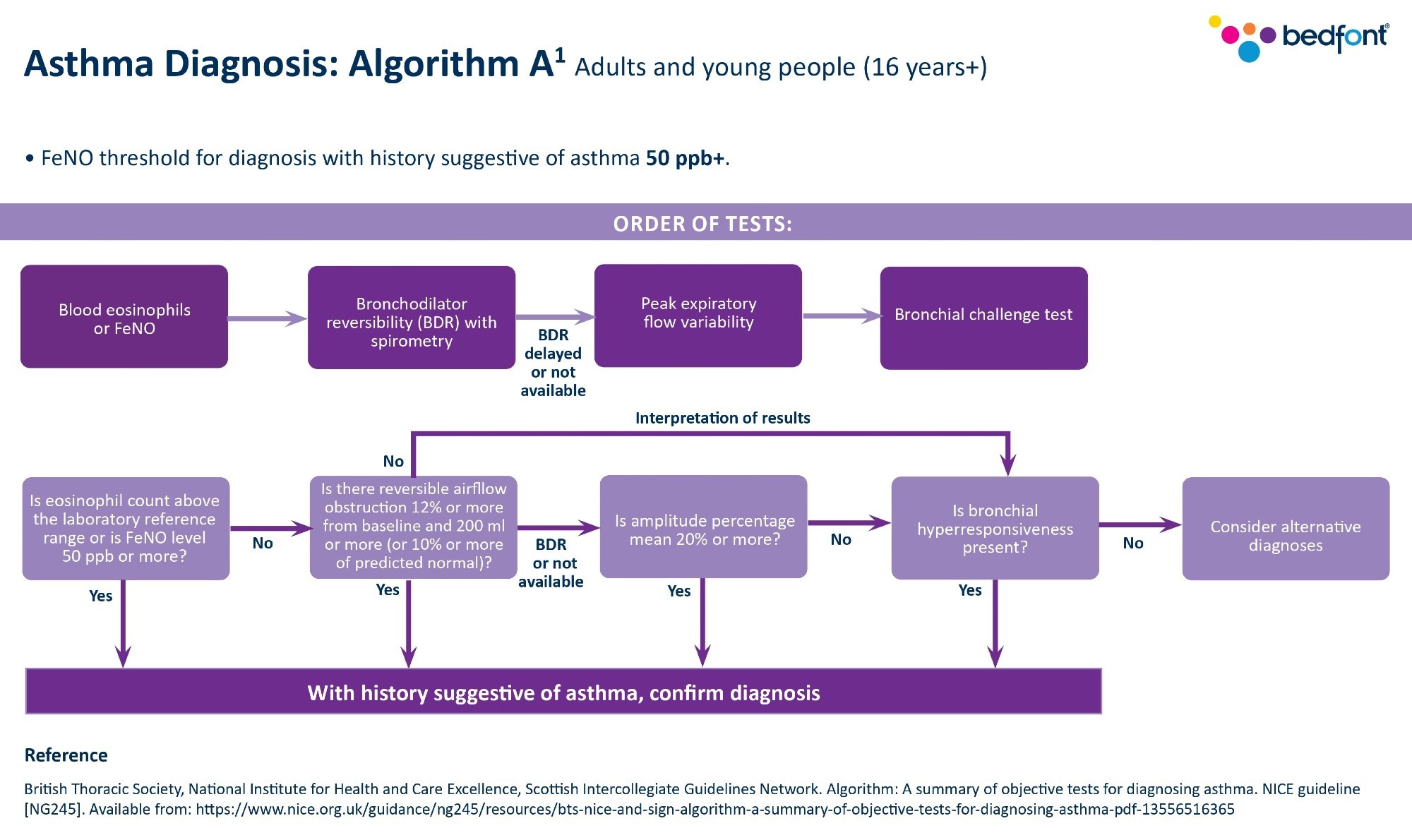
Image Credit: Bedfont® Scientific Ltd
About Carol Stonham 
Since 1986, Carol Stonham MBE has worked as a registered nurse, shifting from acute hospital environments to primary care by 1990. She currently works at the Gloucestershire ICB and heads the Respiratory Clinical Programme Group, while co-leading the NHSE South West Respiratory Network. Carol also serves as a member of the Bedfont® Medical Advisory Board.

About Intermedical Limited
Intermedical (UK) Limited is a leading specialist supplier of medical diagnostic and therapy equipment in the UK cardio-respiratory healthcare industry. Trusted in respiratory health since 1997, the organization is the exclusive distributor of the Bedfont® NObreath® FeNO device in the UK.
About Bedfont® Scientific Ltd
Bedfont® Scientific has specialised in the design and manufacture of exhaled breath and gas monitoring instruments since 1976.
For medical gas monitoring, their Medi-Gas Check medical pipeline testing range verifies not only the quantity but also quality of gas administered to patients.
Bedfont's breath analysers include carbon monoxide (CO) monitors such as the Smokerlyzer®, used for smoking cessation, and the ToxCO®, used by emergency services, to diagnose CO poisoning.
The NObreath® FeNO monitor provides accurate analysis of airway inflammation for the control of asthma, and the Gastrolyzer® range aids in the detection of gastrointestinal disorders and food intolerances. Quick and non-invasive, breath analysis is the new blood test.
Sponsored Content Policy: News-Medical.net publishes articles and related content that may be derived from sources where we have existing commercial relationships, provided such content adds value to the core editorial ethos of News-Medical.Net which is to educate and inform site visitors interested in medical research, science, medical devices and treatments.